Everything you need to know about newborn stool. Norms of coprogram indicators in children. What should a newborn baby's stool look like? Nutrition related
One of the main problems of parents of babies is the child's stool. Parents always think that it is their child who is doing “this” in a completely different way than required, and they are ready to go through hundreds of studies in order to find non-existent problems. Two problems - constipation and diarrhea - are sometimes caused by parents themselves. However, absolutely normal “major results” of a child’s life activity are often considered a problem. To be able to distinguish normal stool from problematic stool, you need to know the norms. Let's talk about them.
Infant chair
The stool of children of different types of nutrition differs significantly in quality and appearance. Therefore, you cannot compare the contents of diapers for a baby and an artificial baby. Due to fully digestible nutrition of ideal composition, infants very rarely have problems with stool only in the case of real illness. By definition, breast milk cannot cause any digestive problems. However, it is these children who have the most imaginary problems.
The biggest questions are raised by the number of bowel movements a child has: usually from 8-10, almost after every feeding, with a volume of about a teaspoon, to once every 5-7 days, but in a larger volume. This phenomenon is called physiologically rare stool; it occurs due to the almost complete digestibility of breast milk - there is simply no “waste” left.
It is quite acceptable for stool to appear “watery”, with a yellow color and interspersed with white lumps, stool when farting, or a porridge-like mass. For a baby up to 6-7 months, stool with mucus, lumps, pieces and even greens is quite normal - this is the formation of microflora and the work of enzymes - there is no need to get involved with “therapeutic” measures in this process. If, with any type of stool, the child is cheerful and healthy, smiles, farts well, eats and sleeps, gains height and weight - this is normal and the child has no problems with stool.
What not to do
Many parents, when the baby does not have stool, try to look for constipation in the child and begin to treat it with barbaric methods. I advise you to first try all the “treatment” methods on yourself, and then apply them to your child. It is forbidden to induce stool by inserting a piece of soap, cotton swabs, the tip of a thermometer or other foreign objects into the rectum!
The introduction of soap into the rectum causes irritation and chemical burns of the rectal mucosa, this causes sharp pain in the child, and inflammation of the rectum disrupts its normal functioning.
Inserting thermometers and sticks into the rectum leads to mechanical injury and disruption of the intestinal sphincter apparatus, which can lead to disruption of the coordinated functioning of the intestines and the formation of true constipation. All artificial stimulants suppress the natural urge to defecate, and children stop going to the toilet “in a big way” on their own, only with stimulants. For reflex defecation to occur, it is necessary to create a certain pressure of feces in the lumen of the rectum, which will send an impulse from the rectum to the brain and open the sphincter. It may take several days for the volume to accumulate.
In addition, you should not supplement your child with various drops, teas and infusions - espumizan, smecta, plantex, dill tea - you should not, unless absolutely necessary, interfere with the process of physiological formation of intestinal microflora and the formation of enzyme activity.
How is bowel function established?
After the baby is born and the first cry, its microflora is formed - the baby receives it from the air, from the skin of the mother’s perineum and chest, and this microflora begins to populate the intestines. In the first two to three days of his life, he empties his bowels of meconium, a dark, olive-colored mass similar to glue or plasticine. These are the remains of intestinal epithelial cells and digested amniotic fluid during nine months of pregnancy. When amniotic fluid is swallowed, the baby trains its digestion to work after birth. Meconium has practically no odor; it is very difficult to wash off diapers and the butt. In the first three days it should completely go away and then the nature of the stool will change.
The stool begins to liquefy, becomes more frequent, and heterogeneous inclusions appear in it - liquid, mucus and whitish lumps; its color is also heterogeneous - there may be areas of dark color with yellow fragments, whitish and colorless, watery. Bowel movements may occur six or more times a day. This stool is called transitional, and it means the colonization of the intestines with microflora and the inclusion of enzymes in the digestive process. As the intestinal sections colonize, the stool can take on different appearances and colors due to irritation of the intestinal wall by microbes and the formation of intestinal immunity. In about one to two weeks, the stool begins to return to normal - it becomes homogeneous, mushy, yellow in color, occurs less frequently and ceases to contain impurities and mucus. This is facilitated by exclusive breastfeeding - if the baby is not given pacifiers, bottles or additional food and drink. If this is present, the correct physiological stool will take longer to form.
From the moment lactation is established and the microflora in the intestines settles down, the baby begins to go to the toilet with “mature” stool - this is a bright yellow homogeneous paste with the consistency of thick sour cream with the smell of cottage cheese. This indicates good absorption of milk, although its frequency can vary from several times a day to once every 5-7 days. Such rare stools are normal during breastfeeding. At the same time, the baby’s health is excellent if he has enough milk and there are no additional supplements or supplements. At the age of 2-4 months, there are usually from 15-20 to approximately 50 grams of feces per day. With the introduction of complementary foods, stools begin to take shape, become less frequent and change in character.
Artificial Chair
Typically, stool in bottle-fed children has a thicker consistency, darker color (from greenish to brown), and occurs from several times a day to once every one or two days. If bowel movements occur less frequently, the formula most likely causes constipation or you are not giving your child enough water. On average, children on IV poop 1-2 times a day, the amount of feces is about 30 g. Due to the predominance of rotting processes, the stool contains E. coli and bifid flora, there may be some mucus and whitish crumbs; this indicates that the baby has not yet fully absorbed the fats of the formula, or you have overfed him.
With the introduction of complementary foods, the stool thickens and begins to form into a soft sausage or mush, the color becomes dark brown, there are no impurities in the form of blood or mucus. The frequency of stool is 1-2 times a day.
This is the stool that should ideally be and which reflects the full functioning of the intestines. But there are variants of deviation from the norm that are not considered a pathology, but are very frightening for parents. Then moms and dads demand immediate action from the doctor, which is unnecessary and can only do harm. But how can we understand where “this” came from in the diaper?
Variants of norm and deviation
Often, white lumps similar to curdled milk are found in a child's stool. With good or excessive weight gain, they indicate some excess supply of milk or formula; This happens when a child receives breastfeeding on demand. This is a good sign: there is more than enough milk, it’s just that some amount of protein and fat does not have time to be processed by enzymes and comes out unchanged - a milk residue is formed. But if, with a large number of lumps in the stool, the child does not gain weight well, this usually indicates a deficiency of enzymes (primarily the liver and pancreas), that is, the intestines cannot cope with the digestion of food. In this situation, the doctor may prescribe enzyme preparations during intestinal maturation.
Often, the stool may have a thinner, even watery consistency with foam, be splashy or have a watery edge on the diaper, and have a sour smell. Sometimes such stools pass when gas is released - in small portions. The stool is yellow or mustard in color, unchanged. This condition is called milk imbalance or transient lactase deficiency. If a child receives a lot of milk, rich in milk sugar (lactose) and liquid, then lactase, an enzyme of which there is still a limited amount in the child’s intestines, simply does not have time to cope with the entire amount of milk sugar received. Then part of it enters the intestines and is fermented by microbes into gas and water - this is how excess gas formation and active metabolites appear - including lactic acid, which irritates the intestinal walls and causes increased peristalsis and loose stools. If washing is not thorough enough, irritation of the anal area may occur - it is necessary to use a protective cream. Correcting the situation is quite simple - there is no need to “save” milk, it is necessary that the breasts are always soft. Then the baby will receive hind milk, low in lactose, but higher in calories.
However, often in such a situation, a diagnosis of lactase deficiency is unreasonably made, which does not reflect the true picture. Lactase deficiency is manifested by poor weight gain, which cannot be corrected even with normal breastfeeding. This is a congenital defect of the enzyme or its severe deficiency (although over time the enzymes can mature). There is often an excess of lactose (milk sugar) in mother's milk - this is a genetic feature or a consequence of an unbalanced diet. The diagnosis is confirmed by analyzing stool for carbohydrates, and, of course, monitoring the child’s well-being. And with dietary restrictions and lactase administration, the condition normalizes. There is no need to rush to switch your baby from breast milk to lactose-free formulas - lactose is necessary for the body, therefore, breastfeeding even with lactase deficiency and introducing an enzyme to digest lactose would be correct.
The worst thing for parents is the presence of “green” in the stool, which causes panic or thoughts of the most terrible diseases. In fact, in the vast majority of cases in young children (up to about 4-6 months) this is the norm. In the first months of life, a lot of bilirubin (a breakdown product of hemoglobin) is released with feces; it oxidizes to a greenish tint in air. Hence the “romantic” admixture of greenery. Sometimes it happens that a mature stool is not established in any way and the baby’s stool for a long time has an unsightly appearance: with greenery, lumps and threads of mucus. This happens when the baby is malnourished, inactive sucking and other problems - hungry stool. Another reason for such stool is the predominance in a woman’s diet of raw fruits and vegetables with a lack of meat, during hypoxia during childbirth. Then the mucous membrane takes longer and more difficult to restore, and the enzymes mature later.
What should mom do?
First of all, you need to remember the rule - if nothing bothers the child and there are no painful manifestations, he has the right to any stool. Even infants can have a long period of stool formation due to difficult childbirth or the establishment of full breastfeeding. The body is a complex system and everyone has an individual development program; you cannot force everyone to fit a single standard. If a child gains at least 500 g per month, urinates well and often, and there are no painful manifestations, this means that this is his normal stool, no matter what impurities are in it, and there is no need to interfere with the delicate process of adjusting the intestines.
Medicinal correction measures must be used if the child is experiencing severe pain, he screams and presses his legs to his stomach, and the stomach itself is tense; if he has rashes, itching and problems with weight and height. It is necessary to consult a doctor, conduct an examination and scatological examination of stool, and adjust the mother’s diet. But stool testing for dysbacteriosis is an absolutely unnecessary and non-indicative test; conducting it is practically pointless.
What should you really be concerned about?
It is necessary to immediately call a doctor or an ambulance if the child has loose stools (mucous or with pieces) in the presence of fever, vomiting or poor health - these are signs of an intestinal infection, and this cannot be the norm. No medications, except maybe smecta, should be given to the child - self-medication in such cases is deadly, dehydration and convulsions may occur.
It is also necessary to pay attention to the retention of stool in a child on IV for more than 2 days - this indicates constipation and may indicate the need to change the formula or feeding regimen. It is also necessary to pay attention to stool retention in infants with rare urination and highly concentrated urine.
In addition, the appearance of a stool in a baby or artificial baby that resembles a dense sausage or “sheep’s balls” requires the intervention of a doctor - these are also manifestations of constipation that require correction.
Particularly dangerous is the appearance of blood, scarlet or coagulated, in the stool. Sometimes small streaks of blood appear when farting with straining due to a crack in the anus. However, these should be isolated and very rare phenomena. The constant presence of blood in the stool can be caused by a number of diseases: allergies and problems with the rectum, infectious diseases and even malformations of the anus.
All parents treat the health of their child with special care. Any changes bring a lot of anxiety. Even after finding grains in a baby’s stool, some may experience real panic when there is practically nothing to worry about. In order for mothers to be calm and react correctly to changes in their baby’s stool, it is necessary to consider a number of the most common problems associated with feces in infants.
Fecal abnormalities in infants
Streaks in baby's stool
When zealous parents discover bloody streaks in their baby's stool, the only thing they want to do is call an ambulance. At the same time, the baby is very active, gaining weight well, his tummy does not bother him and the tests are quite normal. Streaks of blood in the stool of a completely healthy child may appear due to intolerance to the proteins contained in cow's milk. In order for the streaks in the stool of a breastfed baby to disappear, the mother must stop consuming dairy products and the baby’s stool will be restored.
Leukocytes in infant stool
The baby's health is normal if the leukocytes are in the range from 8 to 10. When the leukocytes in the baby's stool exceed the norm, this may indicate a number of problems. Among the most common:
- Dysbacteriosis.
- Ulcerative colitis, studies show an increased number of neutrophils.
- Follicular enteritis. Elevated leukocytes in the feces of infants provoke the appearance of mucus.
- Constipation or spastic colitis.
- Dysentery. The number of neutrophils is greatly increased, bowel movements are very frequent and liquid. Severe intoxication of the body occurs.
- Allergic colitis. Along with the increased number of white blood cells, there is a sharp increase in the level of eosinophils.
When the leukocytes in a baby's stool are very high, a change in its consistency, smell and quantity of stool is observed.
Staphylococcus in the stool of a baby
There is no need to worry about the fact that staphylococcus is present in small quantities in a baby’s stool. It appears even in absolutely healthy babies who did not have any problems in the first weeks or months of life. Staphylococcus may be accompanied by constipation, increased gas formation, and colic. Often the baby cannot go to the toilet on his own. No special treatment is needed. It is worth balancing the mother’s diet, increasing the child’s physical activity, increasing the number of belly rubs, and giving regular tummy massages. Staphylococcus in a baby's stool indicates dysbacteriosis, which can and should be dealt with. Especially in the first stages of life.
Carbohydrates in infant stool
In order to prevent lactase deficiency in babies in the first year of life, carbohydrates in the baby’s stool should be determined. Thanks to this analysis, it is possible to identify the ability to digest and absorb fats and sugars of natural origin. The main reason for the inability to accept fats and sugars of animal origin is the underdevelopment of the gastrointestinal tract or dysbiosis that develops in infants in the first months of life.
The fewer carbohydrates in feces, the better the baby’s body functions.
Black in baby's stool
Sometimes various inclusions may appear in a child’s bowel movements. Black in the stool of a fully breastfed baby appears due to insufficiently absorbed calcium. For children already receiving complementary foods, a similar phenomenon is typical after consuming flour products with poppy seeds, kiwi or banana.
There is no need to worry about the fact that black in the baby’s stool is the result of internal bleeding. Such deviations are typical only for adults. In addition, the speed of food passing through the esophagus is very high, which is why the blood does not have time to darken.
Lumps in baby's stool
Pediatricians consider it quite normal if white lumps are observed in a baby’s stool. Often, if such impurities appear, the reason is very banal: overeating. The baby is put to the breast on demand and the entire amount of food does not have time to be absorbed.
Red in baby's stool
The reason why red appears in a baby's stool may be dysbacteriosis and some other gastrointestinal diseases. In this case, blood can appear either with every bowel movement or quite rarely.
If the red in the baby’s stool does not in any way resemble bloody spots, then the reason may be the red foods consumed by the nursing mother: beets, pomegranates, tomatoes. If the baby is already receiving complementary foods, then the reason lies in new dishes with a red color that are not completely processed during passage through the esophagus.
Grains in baby's stool
If grains appear in the baby’s stool, then there is no need to worry about this. Often the cause of their occurrence is: overfeeding, insufficient absorption of calcium or improper nutrition of the mother.
Fat in baby's stool
As a result of the immaturity of the pancreas, fat is observed in the feces of infants. Most often, such stool occurs in infants who were born prematurely or have abnormalities in the process of intrauterine development. In some cases, similar bowel movements occur in children with various diseases of the liver or biliary tract.
Protein in baby's stool
Quite often, protein in a baby’s stool appears during the course of inflammatory diseases in the baby’s intestines. Additional reasons why the protein norm increases may be putrefactive dispersion or ulcerative colitis.

Clostridia in infant stool
It is worth paying special attention to the fact that clostridia were found in the feces of infants. Often the cause is intestinal dysbiosis, which occurs against the background of an increased amount of protein. If dysbiosis itself is not very dangerous, then the diseases to which it can lead are very alarming. Clostridia in the feces of an infant can lead to putrefactive dispersion, tetanus, botulism, necrotic enteritis, or the presence of an anaerobic infection.
Foam in baby's stool
It’s too early to panic about foam appearing in a baby’s stool. Almost always, such a reaction occurs to a change in the mother’s diet or the introduction of complementary foods. In addition, during the process of “maturation” of the gastrointestinal tract, various changes can be observed: foam, bloody spots, lumps, etc.
Foam in a baby's stool can also be caused by dysbacteriosis or an infection introduced into the body. If no other impurities are observed against the background of foam and the child feels well, then his body is normal.
Flakes in baby's stool
Almost always, flakes appear in a baby’s stool due to a lack of enzymes capable of digesting incoming food, or rather breast milk. In addition, the baby may have an excellent appetite and absorb more than he can absorb, or the mother may have very fatty milk. Flakes in a baby's stool are a passing phenomenon.
Detritus in infant stool
It is quite normal if detritus is found in the stool of a baby. It is simply a product of the body's work. How well the food is processed is evidenced by detritus. It contains everything that the baby and his mother consumed. The better the baby’s digestive system works, the more crushed the particles can be shown by the corpogram.
Enterococci in infant stool
In the first months of life, enterococci perform a very important function: they help absorb various organic substances. Therefore, if you find enterococci in a baby’s stool that is slightly higher than normal, you should not think about the bad. Quite often, the number of enterococci can be quite high. Against this background, dysbiosis can develop, which subsequently provokes various diseases of the gastrointestinal tract.
In some cases, the main carrier of enterococci is the nursing mother, who transmits them in large quantities through breast milk.
Clots in baby's stool
In small quantities, clots may be present in the stool of an infant from time to time. They can consist of both mucus and blood. In this case, it is necessary to focus on the child’s behavior. If he is bothered by abdominal pain, is irritable, and often cries, then the cause of the clots may be either dysbacteriosis or an infectious disease. A corpogram should be made.
Bilirubin in infant stool
In the first months of life, bilirubin should be present in the feces of an infant, since the bacterial flora of the intestine is not sufficiently developed. Up to nine months, bilirubin is processed into stercobilin. From 9 months, bilirubin should be completely absent. If bilirubin is detected, then its cause may be:
- accelerated intestinal motility;
- lack of bacteria;
- antibiotics;
- tendency to rapid evacuation of feces from the intestines.
If bilirubin in the feces of an infant is present in minimal proportions, then the risk of developing or having diseases is very low.
Klebsiella in baby's stool
If the corpogram shows that Klebsiella is present in large quantities in the baby’s stool, then you need to act as soon as possible. Otherwise, along with bloating, dysbacteriosis, constant pain in the intestines, the baby can get a number of rather unpleasant diseases (sinusitis, conjunctivitis, gastrointestinal diseases, pneumonia, meningitis).
Starch in infant stool
Having discovered starch in a baby’s feces, you need to carefully examine its gastrointestinal tract. Perhaps the reason for the failure of starches to break down is accelerated evacuation of intestinal contents, gastritis, and fermentation dispersion. Over time, pancreatitis may develop. Starch in a baby’s stool is not normal, and the sooner the cause of its occurrence is identified, the better.
Red blood cells in the stool of an infant
Normally, red blood cells should be completely absent in the feces of a baby. Their appearance indicates a number of diseases or bleeding. In this case, along with them, there should also be blood in the baby’s stool.
Bacteria in baby's stool
Often, bacteria in a baby's stool appear against the background of dysbacteriosis. Whatever type of bacteria is detected by the corpogram, timely treatment should be carried out in order to prevent degeneration into a more severe form of gastrointestinal diseases.
Whatever is detected in the baby’s stool, the test results should be examined by a pediatrician and, if necessary, prescribed appropriate treatment. There is no need to look for answers to questions and select medications on your own. In some cases, deviations from the norm, against the background of good health in the child, are only a temporary phenomenon.
With the birth of a child, a mother has a lot of fears related to the baby’s health and proper care for him. These fears are not difficult to allay.
Young parents look at the contents of a baby's diaper with interest and trepidation... Is this a familiar picture? The stool often causes anxiety in the mother and can really tell about the health and unhealthiness of the baby - you just need to be able to “read between the lines,” that is, understand the signs of the body.
Let's get to know the norm
While the baby lives and develops in the mother's womb, it accumulates in his intestines. meconium. It is a homogeneous tar-like mass of dark olive, almost black color, practically odorless. It consists of condensed cells of the intestinal mucosa, amniotic fluid swallowed by the baby, etc. Normally, meconium begins to be released from the baby’s intestines after birth and is therefore also called original feces(sometimes meconium is excreted in utero: if the course of labor is unfavorable or at the very end of pregnancy, oxygen starvation of the fetus causes premature bowel movement, in this case meconium enters the amniotic fluid and turns it green). The baby's stool is usually represented by meconium in the first two or three days, that is, until the mother produces a large amount of milk. Sometimes it happens that after the bulk of the meconium has passed, say, during the first day, until the mother’s milk arrives, the baby may not have any stool at all. This is due to the fact that the colostrum, which the baby eats in the first few days, is absorbed by the body almost completely, so that there are no toxins left in the intestines - therefore, there is simply nothing to be excreted.
After the mother has established active lactation, the baby’s stool gradually becomes mature, usually passing through a transitional stage. Transitional is called a stool that combines the features of original feces and mature stool; it has a mushy consistency, yellow-green color and a sour odor. Mature the stool is distinguished by its pure yellow color, homogeneous mushy consistency (it is often compared to thin sour cream), and the smell of sour milk. Its frequency is higher, the younger the child: in the first weeks after birth, bowel movements can occur almost after every feeding, that is, reach 5-8, and sometimes 10 times per day.
Gradually, stool is reduced to approximately 1-3 times a day, but there is a rare variant of the norm when mother’s milk is so completely absorbed by the baby’s body that almost no undigested residue accumulates in his intestines. In this case, bowel movements can occur once every few days, sometimes even once a week. This is due to the fact that only sufficient filling of the large intestine with waste (undigested food debris) is a signal for contractions of the intestinal walls, leading to emptying. That is why the intestines must first “accumulate” the remains in order to then throw them out. As a rule, this feature of the absorption of mother's milk becomes obvious in babies no earlier than 1.5-3 months. Let's make a reservation: the frequency of stool once every few days can be considered normal only if three conditions are met: with completely natural feeding (that is, the baby does not receive anything other than mother's milk), age of at least 1.5 months and the absence of any signs of ill health - pain and bloating in the abdomen, discomfort and difficulty during bowel movements - that is, when the baby eats well, gains weight correctly and nothing bothers him.
Stool during artificial or mixed feeding may be no different from normal, mature breastfeeding stool, or may have a more “grown-up”, putrid odor, thicker consistency, and a darker, brownish color. Bowel movements during mixed or artificial feeding should occur at least once a day; anything else is considered constipation.
Now that we have become familiar with the “ideal” course of the process, it is necessary to become familiar with possible deviations from this.
Greens in the chair
It often happens that the “correct” type of stool is not established for a long time, and even against the background of active lactation in the mother, the stool for a long time retains the features of a transitional one, that is, it has a clear greenish tint, sometimes mucus is also found in it. There are several reasons for this.
- Malnutrition(the so-called “hungry” stool). This often occurs due to a lack of milk from the mother. Factors that make it more difficult for a baby to “extract” milk from the breast can also be flat and inverted nipples and tight breasts, especially after the first birth.
- The predominance of fruits and vegetables in the diet of a nursing woman in comparison with other products.
- Inflammation of the intestinal mucosa in a baby. A very common reason for this is fetal hypoxia (oxygen starvation) experienced during pregnancy and/or childbirth. This pathological condition affects many tissues in the body, including the intestinal mucosa, which then takes quite a long time to recover. In addition, inflammation of the intestinal mucosa can be caused by the influence of synthetic substances - flavors, dyes and preservatives and any artificial compounds present in the mother's diet, penetrating into breast milk and affecting directly the intestinal mucosa, i.e. the mother's consumption of products containing synthetic additives: sausages, smoked meats, all types of canned food, industrial juices, dairy products with fruit and other aromatic fillers. Finally, a very common cause of intestinal inflammation is a disruption of the normal intestinal microflora - in other words, intestinal dysbiosis (or dysbiosis), when representatives of the normal microflora become few, but so-called opportunistic microbes multiply, that is, pathogens that, under unfavorable conditions, can cause inflammation in the intestines. In this case, the mucous membrane suffers as a result of the influence of opportunistic microorganisms and their metabolic products. The risk of development increases significantly if the mother and/or baby were prescribed antibacterial drugs.
What to do? If there is greenery in the stool, the first thing to do is to rule out malnutrition in the baby. Of course, in addition to stool disorders, other symptoms will be noted: the baby may show dissatisfaction at the breast, if milk is poorly released from the nipple, he does not fall asleep after feeding and / or never stands more than 1-1.5 hours between feedings, he has the rate of weight gain and growth is reduced. With severe malnutrition, the number of urinations may decrease in a child (normally it is at least 6-8 per day), urine may be more concentrated (normally it is almost colorless and has only a slight odor). Next, you should act according to the situation: if lactation is insufficient - switch to feeding “on demand” or “at the first cry”, put the baby to the breast more often, allow him to stay at the breast as much as he wants, give both breasts at one feeding, be sure to feed breastfeeding overnight, take medications that stimulate lactation. If the cause of malnutrition lies in the irregular shape of the nipples, it may be worth using special nipple shields during feeding. In any case, if you suspect your baby is malnourished, it is better to contact your pediatrician, as well as a lactation consultant.
With artificial feeding, constipation is much more common.
Next, you should carefully check your mother’s diet. All products containing synthetic additives are subject to unconditional exclusion. We should not forget that often the cause of intestinal inflammation in a baby can be synthetic vitamin preparations taken by the mother (including for pregnant and lactating women), so it is necessary to exclude their intake. You should also make sure that the amount of fruits and vegetables in the diet does not exceed other products (these “gifts of the earth” contain a large amount of acids, an excess of which in breast milk can cause inflammation of the mucous membrane in the baby’s intestines).
Now that we have created all possible prerequisites for proper nutrition of the baby, we should be guided by his well-being. If the baby is gaining good height and weight, he is not bothered by abdominal pain and allergic reactions, he is generally healthy and cheerful, and is interested in the world around him according to his age, then the only symptom - the green color of the stool - can be ignored: most likely he will reflect the consequences or presence of intestinal dysbiosis in the baby. In the human body, especially one that has recently been born, everything proceeds according to its own laws and at an individual speed. Colonization of the intestines with the “right” microbes is not a process of one day or even one week, so even in completely healthy children, transitional stool can persist for up to a month or even more. If this does not interfere with the baby’s normal development, you can not interfere with this process. Still, no drug has yet been created for dysbiosis better than breast milk. The only thing that doesn’t hurt to do if there are lingering signs of dysbiosis is to submit the mother’s milk for culture to make sure that it does not contain pathogenic microbes (if any are detected, their sensitivity to antibacterial drugs must be determined, then the mother is treated with the most effective antibiotics for this case - During this period, breastfeeding is usually stopped).

If not everything is fine in the baby’s well-being (for example, he is tormented by intestinal colic, or skin allergic reactions are noted, or he is not gaining enough weight and height), then you should take some tests - a coprogram and a stool flora analysis (or, as they say , for dysbacteriosis). The coprogram will show how the digestion processes are progressing in the intestines and can confirm the presence of inflammation of the mucous membrane (this will be indicated by an increase in the number in the stool, a sharply acidic reaction, and the presence of hidden blood). In a flora analysis, the main attention should be paid to the presence and/or quantity of pathogenic microorganisms - those that should not normally be found in the intestines or the number of which should not exceed certain limits. The number of “friendly” microbes may be completely indicative if the stool is analyzed later than two hours after collection. Since this is exactly what happens in the vast majority of cases, you don’t need to pay much attention to the number of normal microbes in this analysis. The detection of pathogenic (disease-causing) microbes (provided that the mother's milk has been analyzed and the mother has been treated, if necessary) is the reason for prescribing special medications to the baby. As a rule, treatment is carried out with phages - special viruses that destroy a certain type of pathogenic microbes and do not affect the flora as a whole. In some cases, antibacterial drugs may be prescribed, taking into account the sensitivity of pathogenic bacteria to them. Treatment is completed with drugs that help restore normal microflora.
White lumps in baby's stool
Sometimes you can see white lumps in the baby’s stool, as if someone had mixed coarse cottage cheese into it. If this symptom is noted against the background of normal physical (gaining weight well and growing), then it is evidence of some overeating: the body receives more nutrients than it needs to satisfy real needs (when the breast is offered not only to satisfy hunger, but also any reassurance). There is absolutely nothing wrong with this, since the baby’s body is perfectly adapted to such “overkill”: it simply throws out the excess in the form of such undigested white lumps. Nowadays, when the policy of feeding “at first cry” has been taken, most healthy children at least from time to time have this feature of their stool. If this symptom is accompanied by a lack of weight or height, especially if this lag worsens, most likely there is an enzymatic deficiency of the digestive glands, which does not allow the incoming nutrients to be properly digested. In this case, a pediatrician or gastroenterologist may prescribe enzyme replacement therapy.
Sometimes you can see white lumps in your baby's stool.
Lactase deficiency
Quite often, parents may encounter that the baby’s stool is liquefied, watery, sometimes foams, has a sharper sour smell, and in some cases a changed color - mustard or greenish. On a cotton diaper, such feces leave a water zone around it. Often, stool is passed in small portions even when gas is passed. An acidic stool reaction often causes persistent bowel movements. This picture is observed when the digestion of lactose - milk sugar is impaired, when for some reason the amount of lactose entering the intestines with mother's milk exceeds the amount of the lactase enzyme necessary for its digestion. This can either be due to an excess of lactose in milk (hereditary predisposition of the mother , an excess of fresh milk and dairy products in her diet), or with reduced production of lactase by the baby’s digestive glands. Undigested carbohydrates “pull” a large amount of water into the intestinal lumen, which is why stool has a liquefied, watery character.
Often, lactase deficiency is accompanied by intestinal dysbiosis: the acidic reaction of intestinal contents prevents the colonization of the intestines with the correct flora, and the lack of the required amount of beneficial microorganisms, in turn, reduces the ability to digest carbohydrates. If this does not interfere with the baby’s development (as we have already said, its signs are normal growth and weight gain, the absence of intestinal colic and persistent diaper rash), this condition can be left without treatment. In the vast majority of cases, lactase deficiency is a transient problem and disappears without a trace with age (by about 9-12 months, the activity of the digestive glands increases so much that the baby’s body can easily cope not only with fermented milk products, but also with fresh milk). Severe and lifelong disorders of lactase production are almost always genetically determined: I should think about this type of hereditary disease if close relatives in the family suffer from lactase deficiency in adulthood. To confirm the diagnosis, in addition to a scatological examination, a stool test for carbohydrates is performed. If lactase deficiency is confirmed, the mother should first adjust her diet: exclude fresh milk; if this step is ineffective, significantly reduce the amount of fermented milk products (the exception is cheese, which contains virtually no milk sugar). If all of these measures fail, your doctor may prescribe lactase replacement therapy.
Constipation in infants
Constipation is considered to be the absence of independent stool for more than a day (of course, except in cases of complete digestion of milk), as well as cases when bowel movements are difficult and accompanied by significant discomfort.
Constipation is quite rare during breastfeeding, and there are two main reasons for it: poor nutrition of the mother and impaired intestinal motility, including spasm of the anal sphincter.
Improper nutrition of the mother is expressed by a tendency towards foods rich in proteins and easily digestible carbohydrates, a lack of dietary fiber. Therefore, if constipation occurs in the baby, the mother should first normalize her diet: give preference to cereals (especially buckwheat, brown rice, oatmeal), whole grains bread, include boiled vegetables in the diet. Some products (peaches, apricots, prunes, dried apricots, figs, boiled beets, fresh kefir) have pronounced laxative properties. In many cases, they will normalize not only your own stool, but also the baby’s stool.
If such measures do not lead to anything, most likely there is a violation of intestinal motility (or, on the contrary, a spasm) and/or a spasm of the anal sphincter. When the sphincter spasms, the passage of gases from the intestines is also difficult, so constipation is often accompanied by severe intestinal colic. Unfortunately, it is almost impossible to combat these conditions with home methods, since they are associated with a violation of the nervous regulation of smooth muscle tone and are consequences of birth trauma or an unfavorable course of pregnancy. If they are accompanied by other symptoms that force you to consult a neurologist (excitability or, conversely, lethargy of the baby, sleep disturbances, weather dependence, muscle tone disorders, etc.), then the treatment prescribed by him for problems with the central nervous system often helps to improve the situation with constipation, If, in the absence of stool, the baby is bothered by pain and/or bloating in the abdomen, you can try installing a gas outlet tube, which will allow you to gently stimulate the anus. With artificial feeding, constipation, unfortunately, is much more common, since the digestion of infant formula is a great difficulty for the baby's digestive system. In many cases, the situation can be normalized by replacing half of the baby’s daily diet with fermented milk formula (sour milk formulas can be gradually introduced after 3 weeks of life). After 4-6 months of life, you can introduce decoction and puree of prunes into your baby’s diet, which help cope with constipation in most cases.
02/05/2010 17:07:39, Elena ShAbnormal bowel movements in infants are, of course, a serious cause for concern. Mucus in stool – pathology or normal? When is medical help needed? Let's figure it out together.
Development of the gastrointestinal tract from birth. What does a normal stool look like?
After birth, the baby's first stool looks like a homogeneous dark green mass - this is meconium. After 3-4 days, the stool becomes noticeably thinner, and the number of bowel movements increases. At this time, the natural colonization of the intestines with bacteria begins. Let us remember that initially it was sterile. During this period, most infants may notice elements of mucus in their stool, but this does not pose any danger.
2-3 days later, stool characteristics will begin to depend on the type of feeding. If a mother breastfeeds her baby, the stool turns yellow (orange), resembles sour cream in consistency, and acquires a sour smell. The formation of the gastrointestinal tract continues, so milk may not be completely absorbed. White grains appear in the stool, which is normal and can last for several months.
The frequency of bowel movements is a purely individual value, but a certain pattern can be traced. So, up to 2-3 months, the baby can poop after each feeding, up to six months - on average, 3 times, and after this age - 1-2 times a day.
If the baby eats formula, the picture will be different. After passing meconium, the stool becomes very dense and light yellow in color. The average frequency of stool in “artificial” patients is initially 1-2 times a day. With the introduction of complementary foods, the feces thicken, darken, and the smell becomes typical.
Mucus in stool: dangerous or not?
The presence of mucus in feces as such is not an anomaly, especially during the newborn period, when the body adapts to new conditions. Mucus serves as protection for the intestines from damage (mechanical and chemical). Stools with mucus are light in color and become softer in consistency. However, the mucus should be mixed with the feces, this makes it invisible. If its inclusions can be seen without much difficulty, adults should not ignore this body signal.
Watch your baby's stool for a while. If this is a rare occurrence, it usually does not mean anything terrible. But if it appears systematically, there are accompanying symptoms (anxiety, weight loss, poor appetite, etc.), you cannot do without consulting a doctor.
Possible reasons
Nutrition related
1. With natural feeding. The mother needs to streamline her own diet. The baby's body can react this way to certain foods. For example, for sweet, fatty, flour or fried. It is necessary to exclude all harmful and questionable foods and from now on adhere to a special diet for nursing mothers.
If, after normalizing the diet, mucus impurities have not disappeared, the mother can have her milk tested to determine whether it is sterile. In rare cases, it happens that the analysis gives a positive result. Next, you need to follow the instructions of the doctors.
2. With artificial feeding. Perhaps the chosen formula is not suitable for the child (there is an allergy, some component is poorly digested). Moreover, in some cases, a cumulative effect appears. At the beginning of taking the mixture, the body does not show its “dissatisfaction” in any way, but then it becomes increasingly difficult for it to process the product, and it lets you know about it. When choosing or changing a mixture, it is better to consult a pediatrician or gastroenterologist. Remember that you cannot suddenly switch your baby to a new product. Sometimes it is advised to continue feeding the baby the same way, but replace one of the daily feedings with fermented milk formula.
3. Reaction to the introduction of complementary foods. Already at 4-6 months, babies begin to expand their diet with complementary foods. Previously, it was advised to start with juices, then give fruit and vegetable purees, and then porridge. Modern pediatrics looks at this issue differently. It is recommended to start with cereals (introduce gluten-free ones first), then start giving vegetable purees, then fruit purees. Juices should not be introduced early; their nutritional value is too exaggerated. There is no valuable dietary fiber, but there are fruit acids and a fairly large amount of sugar.
Each new product should be introduced little by little, gradually increasing the portion. If this rule is neglected, you can overload the digestive system, and then mucus will appear in the stool. This reaction is also possible to a certain product or type of product (most often fruits or vegetables).
To help, you need to reduce the amount of the new dish, the speed at which it is introduced into the menu, or stop giving it altogether for now.
4. Individual intolerance to a specific dish. There is only one way out - to exclude the product that irritates the intestines from the child’s diet.
5. Irrational nutrition. Long intervals between feedings, larger portions than needed, lack of water - all this can cause fermentation and other troubles. The appearance of mucus is just one of the possible consequences.
When it's not about nutrition
Incorrect feeding is relatively easy to correct, so with proper attention, the baby’s stool quickly returns to normal. Unfortunately, it happens that the problem is the development of pathology. It could be:
1. Intestinal infection(dysentery, salmonellosis, rotavirus). Then, in addition to mucus in the stool, there are also signs:
- vomit;
- temperature increase;
- lack of appetite;
- lethargy;
- pale skin;
- changes in color, smell, density, number of bowel movements per day.
If adults notice such symptoms, they should call a doctor. Sometimes hospital treatment is required.
2. Lactase deficiency. Lactase is an enzyme necessary for the processing of lactose (milk sugar). A baby may lack it from birth, and it is also destroyed under the influence of pathogenic microorganisms if there are too many of them. The result is dyspeptic symptoms: flatulence, stool disorders, abdominal pain, inability to completely digest food (the presence of white lumps and mucus in the stool).
Enzyme deficiency is detected by analyzing stool for carbohydrate content. Therapy consists of a therapeutic diet and taking lactase medications; when feeding a child with formula, a lactose-free option is selected.
3. Celiac disease(gluten intolerance). This is the inability to process gluten and some other grain proteins. Such proteins remain unprocessed, causing an autoimmune reaction, resulting in intestinal damage. Symptoms may vary: bloating and abdominal pain, vomiting, low weight gain, bowel changes (including mucus), iron deficiency, anxiety. The basis of treatment is a special diet and replenishment of missing enzymes by taking medications.
4. Dysbacteriosis. Disruption of the natural balance of microflora is one of the most common causes of stool problems in infants. This is when pathogenic and opportunistic microorganisms predominate over beneficial bacteria. Primary signs: flatulence, constipation, mucus in the stool. In advanced cases, there is diarrhea, white flakes, an abundance of mucus and other impurities are visible in the stool. The diagnosis is made based on test results and the collected medical history. The treatment is quite long, it involves sanitizing the intestines, taking probiotics and correcting nutrition.
5. Intussusception. The most dangerous of the reasons, requiring immediate medical attention. The disease is characterized by obstruction in a certain part of the intestine when it is compressed by another part of the intestine.
The symptoms are quite clear:
- severe abdominal pain during and after feeding;
- frequent, severe fountain vomiting;
- the stool has the following features: at first, the feces are diarrhea mixed with blood and mucus, then it becomes like clots of mucus streaked with blood.
Treatment requires surgery. Delay in providing assistance is dangerous for the health and life of the baby.
6. Atopic dermatitis. This disease is hereditary and depends on the characteristics of the immune system. If skin rashes are visible to the naked eye, then many are not even aware of the possible damage to internal organs. Their mucous membrane suffers, and fragments of mucus may appear in the stool.
Also, mucus in a baby's stool may be a reaction to certain medications. For example, for drugs based on simethicone (“Bobotik”, “Espumizan”, etc.). If the problem is due to medications, after the end of therapy the symptom disappears on its own.
The appearance of mucus as a source of information
Its color can tell you something about the possible reasons for the appearance of mucus in stool:
- transparent - inflammation of the respiratory system, or the intestines are attacked by enteroviruses;
- white – the presence of helminths, polyps or intestinal pathologies, it is important not to delay the examination;
- green – the result of the activity of harmful bacteria, medical attention is required;
- yellow – intestinal dysfunction, helminths, enzyme deficiency;
- red (pink) – traces of blood, it is necessary to urgently show the baby to a doctor.
When to call an ambulance:
- stools are loose, too frequent, foul-smelling, and contain impurities that look like blood;
- at the same time, the baby is restless or, on the contrary, too lethargic;
- there are any other warning signs (for example, atypical behavior, vomiting, hyperthermia, pallor, refusal to eat).
Be attentive to your child, contact medical professionals in a timely manner, then many problems can be avoided. Health to you and your baby!
Every mother instinctively worries that her child is protected, warm and fed. The woman looks for confirmation that the baby is eating properly and is not experiencing digestive problems in diapers and a potty. And if she discovers something strange there, she runs to the clinic to take a general stool test for the child. How to understand from a coprogram when to worry, and what indicators are normal?
The essence of scatological research
Stool analysis includes a macroscopic examination of the sample to determine consistency, color, odor and large inclusions, as well as microscopic examination of the contents and biochemical tests. Microscopy reveals mucus, starch, undigested food particles, protein and many other components of stool. A scatological examination helps to recognize various abnormalities in the functioning of the digestive system. This analysis is especially important in early childhood, when any disturbances in the body can affect the overall development of the child.
 It is based on the results of the coprogram that dangerous hereditary diseases associated with insufficient production of digestive enzymes necessary for the breakdown of disaccharides can be identified in the first year of life. Such pathologies include, for example, cystic fibrosis (damage to the exocrine glands) and celiac disease (congenital inability to break down gluten). To clarify the diagnosis, a stool test for trypsin, a pancreatic enzyme, is sometimes prescribed. Parents should not ignore routine screening tests of stool, urine and blood, even if the child appears to be quite healthy. Such studies help to identify pathologies at an early asymptomatic stage.
It is based on the results of the coprogram that dangerous hereditary diseases associated with insufficient production of digestive enzymes necessary for the breakdown of disaccharides can be identified in the first year of life. Such pathologies include, for example, cystic fibrosis (damage to the exocrine glands) and celiac disease (congenital inability to break down gluten). To clarify the diagnosis, a stool test for trypsin, a pancreatic enzyme, is sometimes prescribed. Parents should not ignore routine screening tests of stool, urine and blood, even if the child appears to be quite healthy. Such studies help to identify pathologies at an early asymptomatic stage.
Indications for analysis
Children are prescribed a coprogram as planned in the first year of life to assess the degree of maturity of the digestive tract. However, the main indications for conducting scatological examination include the diagnosis of gastrointestinal diseases and assessment of the effectiveness of treatment. Analysis may be needed in the following situations:
- if blood, mucus, or pus are visible in the stool with the naked eye;
- with obvious underweight or weight loss in the baby;
- if the child is restless, cries a lot and has a poor appetite;
- when the baby has an umbilical hernia;
- if the doctor, based on symptoms, suggests the presence of a pathology of the digestive system.
Deciphering the coprogram, normal indicators
A specific feature of childhood is the rather long process of formation and maturation of the digestive system, so the bowel movements of boys and girls are very different from those of adults.
The norms for stool coprogram indicators when deciphering in children are presented in the table:
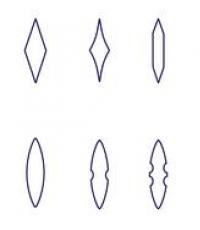
| Indicators | Breastfed infants | Formula-fed infants (IV) | Children over one year old |
| Consistency | mushy | Thick, putty-like | Decorated |
| Smell | Sourish | Smells rotten | Not harsh |
| Color | Green-yellow | Tan | Brown |
| Acidity(pH) | Sour | Slightly acidic | Neutral |
| Blood (erythrocytes) | Absent (-) | (–) | (–) |
| Soluble proteins | (–) | (–) | (–) |
| Detritus | Different volume | Different volume | Different volume |
| Digestible fiber | (–) | (–) | (–) |
| Connective fibers | (–) | (–) | (–) |
| Muscle fibers | A little or not at all | A little or not at all | (–) |
| Slime | In the form of small inclusions | (–) | (–) |
| Starch | (–) | (–) | (–) |
| Bilirubin | (+) | (+) | (–) |
| Stercobilin | (+) | (+) | 75–350 mg/day |
| Neutral fats | Droplets | Small amount | (–) |
| Leukocytes | Single | Single | Single |
When conducting scatology, soaps, ammonia, fatty acids and various crystalline compounds are also detected. For example, Charcot-Leyden crystals indicate allergies, helminthic infestations or amoebiasis. Calcium oxalates indicate low stomach acidity or too many vegetables in the diet. Tripelphosphate crystals during an alkaline reaction of feces are an indicator of increased putrefactive processes in the intestines. The doctor deciphers the coprogram, relying not only on indicators, but also on the clinical picture.
What should a newborn's stool look like?
A newborn baby's feces change very quickly. During this period, it is especially important to monitor the baby’s appetite and weight gain. In the first 3 days, meconium is released - the baby's original feces are dark green and mucous, including bilirubin, epithelial cells, fats, and cholesterol crystals. After this, greenish-brown semi-liquid stools are observed for a week; such stool is called transitional. Over a 4-week period, the baby's stool acquires a characteristic cheesy consistency and an orange-yellow hue. A newborn's feces should be free of any pungent odor or pathological impurities.

Fecal norms in an infant
As the baby develops, his digestive system also matures, which cannot but be reflected in feces. Each baby is individual, capable of defecating from 1 to 6 times a day. And all this is the norm. Until the age of three months, a child develops bacterial flora in the intestines that can convert bilirubin into stercobilin. Until about 9 months, bacteria only partially cope with this task. Therefore, the detection of bilirubin in a baby of this age is considered normal. When starch is detected in an infant's stool, this is most often associated not with gastrointestinal pathology, but with complementary foods, which include vegetable puree from potatoes, bananas and other starch-containing foods. Undigested food particles found in the diaper of a child aged 3–12 months, as a rule, do not indicate digestive disorders. This often happens during teething, overfeeding, poor processing of foods, and early introduction of complementary foods.
When conducting scatology, the decoding of a baby depends on the type of feeding.
For example, with artificial or mixed feeding, the baby’s feces smell unpleasant and smell rotten, this is due to the rotting of casein (cow’s milk protein). Such babies usually defecate less often than those who are fed with mother's milk. Their feces are not acidic, but neutral or slightly alkaline, and microscopy shows a slightly increased content of fatty acids. In an artificial diet, the properties and frequency of bowel movements may change due to a change in the mixture.
With natural feeding, the baby's stool is semi-viscous, yellowish, with fat drops and a sour smell. If feces of an unusual color, white specks, grains of sand, etc. are found in a baby’s diaper, do not immediately worry. It is important to realize one simple thing - a breastfed baby can have stool of any color, consistency and frequency of bowel movements, provided that the general condition is not disturbed, there are no problems with appetite, and the baby is gaining weight normally.
Fecal norms in children over one year old
For a healthy one-year-old child and older, the norm is to go to the toilet from 3 times a day to 3 times a week; the feces are already formed and do not have a strong odor. If irregular bowel movements are accompanied by pain, and the stool is too hard, then we can talk about constipation. The physical properties of children's feces can easily change depending on the foods consumed. Granular stool, for example, is an indicator of a lack of water or fiber in the body.

Normally, after a year, tests for bilirubin, red blood cells and protein should be negative in a child, and positive for stercobilin. Before worrying about the contents of the potty and conducting examinations for dysbiosis and other disorders, it is important to understand that feces do not exist on their own; it must be linked to the child’s condition. If your baby is jumping and jumping, and bowel movements seem strange, you need to calm down and just watch.
Preparing a child for a stool test and rules for collecting a sample
How and how much do you need to collect stool for analysis from an infant or older child? For greater reliability of the study, it is advisable to prepare the baby in advance. The day before, you need to stop taking medications: antibiotics, Smecta, De-Nol, etc. In order for the indicator of occult blood in the feces to be reliable, three days before taking the sample, you should exclude from the diet foods that can increase hemoglobin levels: liver, tomatoes, meat, etc. Preference in nutrition should be given to cereals, and it is better to limit fresh fruits and vegetables.
The algorithm for taking a sample for a coprogram is very simple. It is necessary to collect feces with a special spatula in a dry, clean container, if possible in the morning, immediately before submitting it to the laboratory. In terms of quantity, a teaspoon will be enough.
If you only have the opportunity to collect stool in the evening, it is important to remember that the sample can be stored for no more than 10 hours and only in the refrigerator at a temperature no higher than +5 degrees; it cannot be frozen.
It is better to take feces from a baby not from the diaper, but from the diaper.
Dangerous situations
Certain changes in stool require special attention from parents, even if the baby does not have any characteristic symptoms of illness. Here are some situations in which it is dangerous to delay visiting a specialist:
- Watery diarrhea, which may indicate lactase deficiency, is not so easy to detect in a baby, because the diaper quickly absorbs moisture released in feces. Therefore, if in the first weeks of life a baby produces bright yellow feces with a sour odor more than 8 times a day, it is worth taking a sample for analysis.
- Grayish-white stool in a newborn or older child, due to low levels of stercobilin, may be a sign of hepatitis, bile duct blockage, or pancreatitis. An additional marker of biliary tract pathology is obstructive jaundice. It is worth noting that for a newborn baby, jaundice is the norm, provided that he is gaining weight and does not show much concern. But if the yellow tint to the skin persists after two months of age, the baby must be examined.
- It is urgent to show the child to the doctor if symptoms such as weight loss, bloated abdomen, loose stools are observed, this may indicate congenital enzyme deficiency.
- Dark-colored stool indicates possible bleeding from the upper intestines.
- Visible traces of blood in the stool of a child aged 6 months to 2 years may be a consequence of intussusception, which requires urgent surgery.
Any pathological changes in feces, combined with vomiting and a disturbed general condition, is a reason to immediately consult a doctor.